Alternative Payment Models
Latest Updates
On September 23, ANCOR published its latest white paper on alternative payment models. shares lessons from our work with five emerging alternative payment model programs to discern what works and what lies ahead within this constantly evolving landscape.
What is Value-Based Purchasing (VBP)?
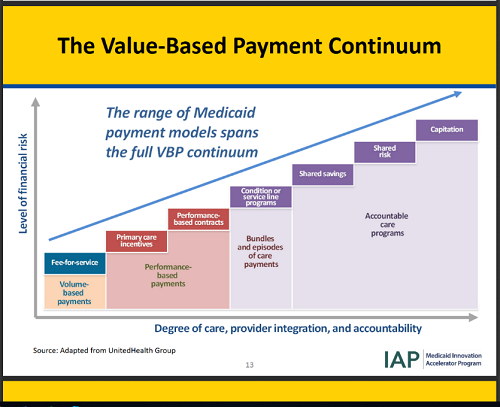
Across the health care industry, improved outcomes and quality of life are key drivers in today’s featured, and tomorrow’s envisioned, health care initiatives. As such, health care payment systems, including Medicaid, are increasingly moving away from fee-for-services and shifting toward paying for value and outcomes which offer the potential for improvements in efficiency, quality, and flexibility in service provision.
ANCOR has been a longtime leader to help “shape, innovate and transition to the emerging environment of long-term services and supports including health care integration,” ANCOR offers this one-stop resource on value-based payment models to guide a thoughtful and deliberate adoption of new approaches in intellectual and developmental disabilities (I/DD) service provision.
As ANCOR shares in its new report on Advancing Value & Quality in Medicaid Service Delivery for Individuals with Intellectual & Developmental Disabilities, value-based purchasing is defined as “any activity a state Medicaid program undertakes to hold a provider or a managed care organization accountable for the costs and quality of care they provide or pay for.”
“Alternate Payment Models” are “a strategy that changes the way Medicaid providers are paid, moving away from fee-for-service payments (which rewards volume), to methods of payment that incentivize value.”
Source: National Association of Medicaid Directors, “Medicaid Value-based Purchasing: What is it & Why Does it Matter?” January 2017
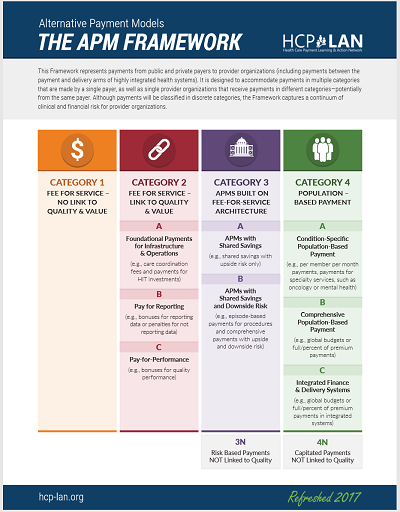
Alternative Payment Models (APM) Framework. July 11, 2017
The Alternative Payment Model (APM) Framework began as a payment model classification system originally presented by the Centers for Medicare and Medicaid Services. The framework was later modified and refined by the Health Care Payment Learning & Action Network (HCP-LAN) work group. The Framework tracks progress toward payment reform and provides a pathway for the delivery of person-centered care. Website: https://hcp-lan.org
Source: Medicaid Innovation Accelerator Program (IAP):
What is the Relevance to the I/DD Field?
 According to ANCOR analysis of the 2018 report on 50-state survey conducted by the Kaiser Family Foundation, quality, value, and outcomes initiatives are key areas of focus for Medicaid. Most recent alternate payment model (APM) initiatives in Medicaid have focused on physical / acute health care services, and increasingly extend to behavioral health and LTSS. The ANCOR Foundation and UCP’s Case for Inclusion 2019 measures outcomes to rank states in their use of Medicaid funds – stakeholders and states use these rankings to determine where to improve services, allocate more resources, and show the successes of their programs.
According to ANCOR analysis of the 2018 report on 50-state survey conducted by the Kaiser Family Foundation, quality, value, and outcomes initiatives are key areas of focus for Medicaid. Most recent alternate payment model (APM) initiatives in Medicaid have focused on physical / acute health care services, and increasingly extend to behavioral health and LTSS. The ANCOR Foundation and UCP’s Case for Inclusion 2019 measures outcomes to rank states in their use of Medicaid funds – stakeholders and states use these rankings to determine where to improve services, allocate more resources, and show the successes of their programs.
The unique needs of individuals with I/DD and their families; the limited nature of approaches to APMs for long-term services and supports (LTSS) and I/DD services; and mixed experiences with transitions of LTSS to commercial, risk-bearing managed care organizations (MCOs) support the belief that any I/DD service transition into this area be undertaken thoughtfully and deliberately.
In January of 2019, ANCOR released its white paper exploring value-based payments in the I/DD field and recommendations for successful models. This is the first report of its kind and has been recognized by national disability organizations, and shared with key agencies in the federal government as a resource guide in our field:
Based upon its yearlong examination of alternate payment models (APMs), ANCOR established 14 payment reform principles to guide the development and assessment of new and emerging APMs for Medicaid I/DD services. It also established 13 recommendations for current and future APMs for I/DD services. ANCOR proposes that the recommendations, principles, and policy analysis included in this report support state efforts in moving toward APMs for I/DD services.
Defining Key Terms
|
Term |
Definition | |
|
Value-Based Purchasing (VBP) |
|
|
|
Alternative Payment Models (APMs) |
|
|
| Capitation |
A payment model in which payments are made based on the numbers of people enrolled or served in the expectation that services are provided rather than being based on the specific services that are delivered. |
|
|
Fee-for-Service Models (FFS) |
Models in which payments are made for a service or unit of service that is delivered, and where payments vary based on unit of service. Fee-for-service includes payments that are made based on time-based billing increments during which the services are provided (monthly, daily, hourly, or half hourly rates). |
|
|
Managed Long-Term Services and Supports (MLTSS) |
|
|
| Social Determinants of Health |
|
Sources:
- National Association of Medicaid Directors, “Medicaid Value-based Purchasing: What is it & Why Does it Matter?” January 2017
- Health Care Payment Learning and Action Network, “Alternative Payment Model Framework, Refreshed for 2017,” July 2017
- Center for Health Care Quality and Payment Reform, “The Payment Reform Glossary: Definitions and Explanations of the Terminology Used to Describe Methods of Paying for Health Care Services,” First edition, October 14, 2014
- Center for Health Care Quality and Payment Reform, “The Payment Reform Glossary: Definitions and Explanations of the Terminology Used to Describe Methods of Paying for Health Care Services,” First edition, October 14, 2014
- CDC Social Determinants of Health (SDOH): Know What Affects Health
Implementation Considerations
Integrated Care
As states consider value-based payment models in I/DD services, they are looking to Managed Long-Term Services and Supports as a mechanism to implement VBP.
Integrated care approaches help states to achieve the following:
- Budget Predictability
- Shift of Risk
- Administrative Simplification (for States)
- Improved Care Coordination
- Utilize quality standards to monitor performance
- Source: What CBOs Need to Know About Managed Long-Term Services and Supports, HCBS Business Acumen Webinar, May 2017
ANCOR is a major partner in a federal grant with the Administration on Community Living (ACL) that builds the business acumen of community-based organizations like I/DD providers to work with states and MCOs directly to lead integrated care model development. The grant funded HCBS Business Acumen Center features a myriad of resources for I/DD providers in this space.
The HCBS Business Acumen Center increases the capacity of disability community-based organizations (CBOs) to most effectively contract and operate in integrated care systems. Specifically, the Business Acumen Center provides business resources, disseminates information, and conducts training to support the development of business relationships between disability CBOs and health plans, integrated health care entities, and other payers to result in positive outcomes for individuals with disabilities.
Website: hcbsbusinessacumen.org
Select Resources:
- White Paper (co-authored by ANCOR and Gold Partner MediSked): Provider Readiness for Operating in Alternative Payment Environments, August 18, 2020
- Webinar: Building the Framework for IDD Quality Measures, January 23, 2019
- Webinar: What CBOs Need to Know About Managed Long-Term Services and Supports, May 24, 2017
There are unique and key issues that must be considered for MLTSS as it pertains to the I/DD services, as outlined in ANCOR’s white paper on MLTSS and guiding principles for MLTSS.
ANCOR’s MLTSS whitepaper provides guidance to all stakeholders on the program design and implementation features that are more likely to result in high-quality, integrated supports that lead to positive outcomes for individuals with I/DD.
ANCOR Principles of Managed Long Term Services and Supports (MLTSS) ANCOR recommends the guiding principles to be rigorously applied in designing and operating Medicaid managed long term services and supports (MLTSS) systems serving children and adults with chronic disabilities
Social Determinants of Health
Resources to guide discussions on defining outcomes.
CDC Social Determinants of Health
Quality Measures
Resources to guide discussions on measuring quality.
National Quality Forum: A National Framework for Health Care Quality Measurement and Reporting
National Core Indicators Survey
CQL: Personal Outcome Measures
Capacity Building Resources
CMS: Medicaid Innovation Accelerator Program (IAP) Value-Based Payment & Financial Simulations function
The CMS Medicaid Innovation Accelerator Program (IAP) functional area of value-based payment and financial simulations offers targeted technical support and solutions to Medicaid agencies in building and strengthening their capacity as they design and implement Medicaid delivery system reforms.
Select Resources:
- Webinar: Medicaid Value-Based Payment Approaches and Key Design Considerations National Learning Webinar October 5, 2017
HCP-LAN: Health Care Payment Learning and Action Network
Launched in 2015 by the U.S. Department of Health and Human Services (HHS), The Health Care Payment Learning & Action Network (LAN) is a public-private partnership whose mission is to accelerate the health care system’s transition to alternative payment models (APMs) by aligning the innovation, power, and reach of the private and public sectors. The LAN’s purpose is to facilitate the shift from the fee-for-service (FFS) payment model to a model that pays providers for quality care, improved health, and lower costs.
Website: https://hcp-lan.org
Select Resources:
- White Paper: Alternative Payment Model (APM) Framework, July 11, 2017
ReThink Health: http://RethinkHealth.org
Funded by the Rippel Foundation, ReThinkHealth was launched by some of the nation’s most influential leaders in health, economics, politics, business, and energy to reimagine and transform health.
Website: www.rethinkhealth.org
Select Resources: