Capitol Correspondence - 04.11.23
First States Begin Medicaid Redetermination Process Following COVID-19 PHE Unwinding

Share this page
Stay Informed on the Latest Research & Analysis from ANCOR
More News
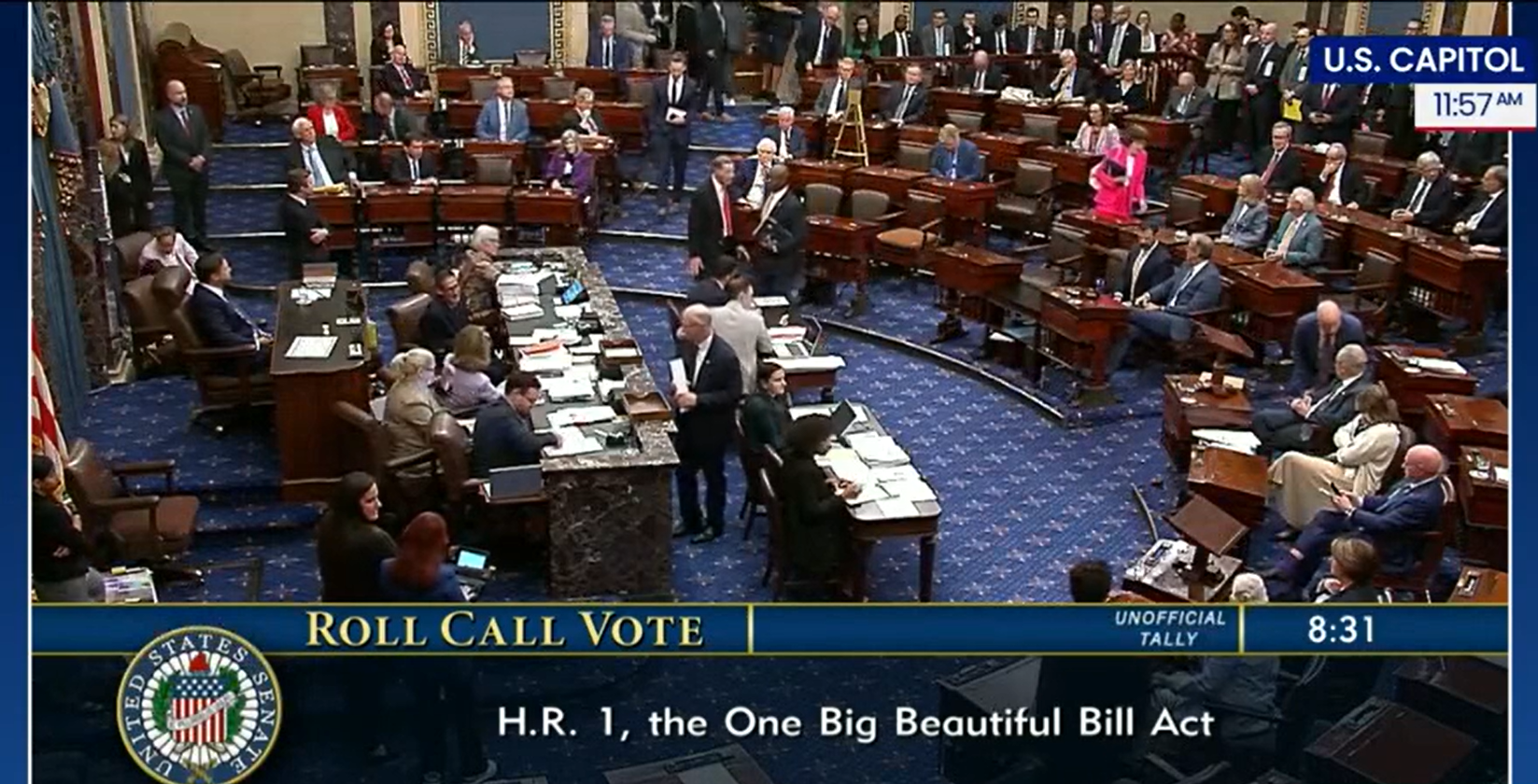
Press Release - 07.03.25
Statement on Final Passage of the Republican Reconciliation Package

Capitol Correspondence - 07.01.25
U.S. Supreme Court Issues Decision to Limit Nationwide Injunctions