Connections - 06.01.23
Key Elements of Psychotropic Stewardship Promote Responsible, Appropriate Prescribing
Share this page
Stay Informed on the Latest Research & Analysis from ANCOR
More News
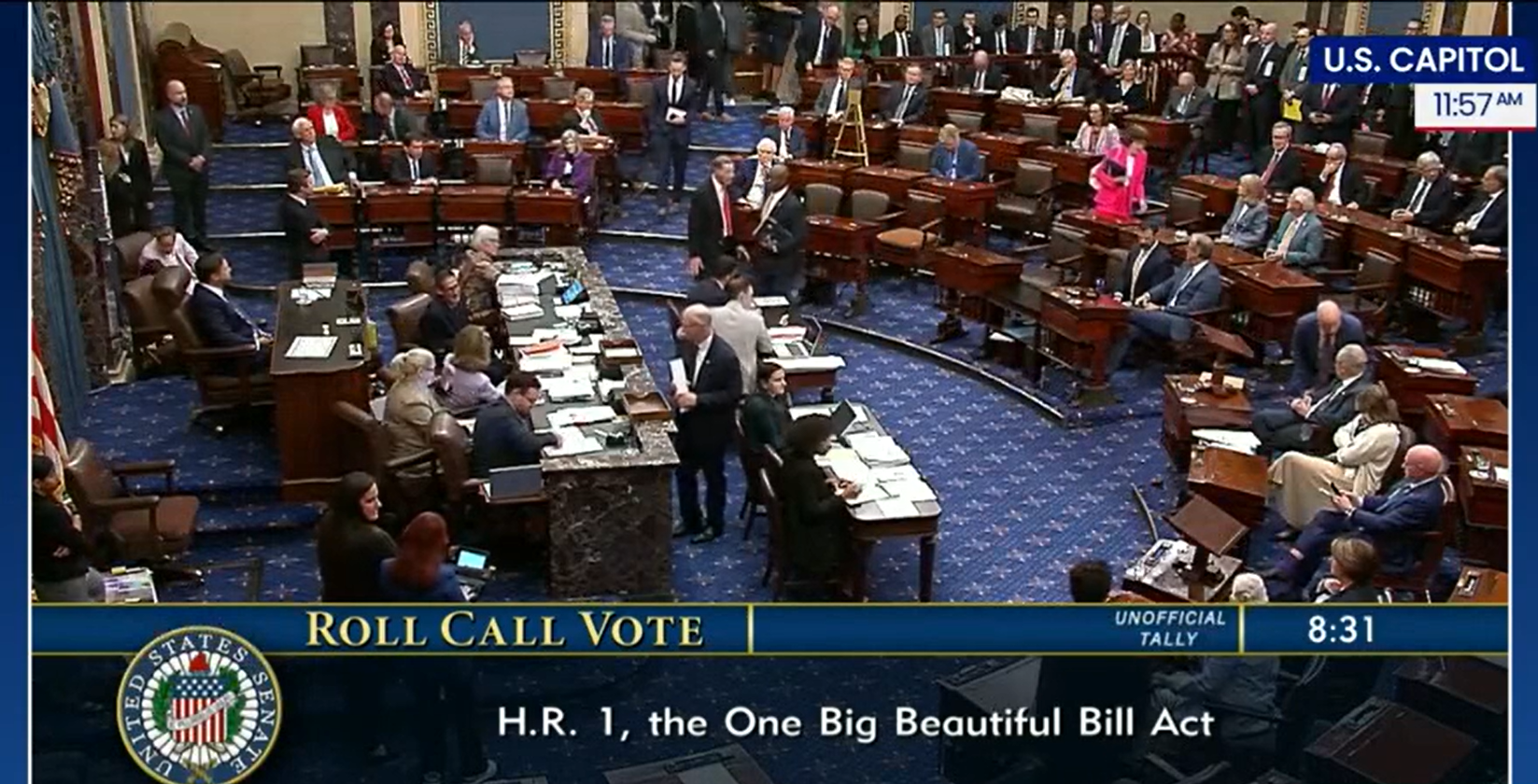
Press Release - 07.03.25
Statement on Final Passage of the Republican Reconciliation Package

Stateside Report - 06.23.25
Stateside Report: June 30, 2025