Connections - 05.31.21
Wait List Management: Challenges and Solutions to Improve Outcomes
Share this page
Stay Informed on the Latest Research & Analysis from ANCOR
More News
Stateside Report - 06.23.25
Stateside Report: June 30, 2025

Stateside Report - 06.23.25
Stateside Report: June 23, 2025



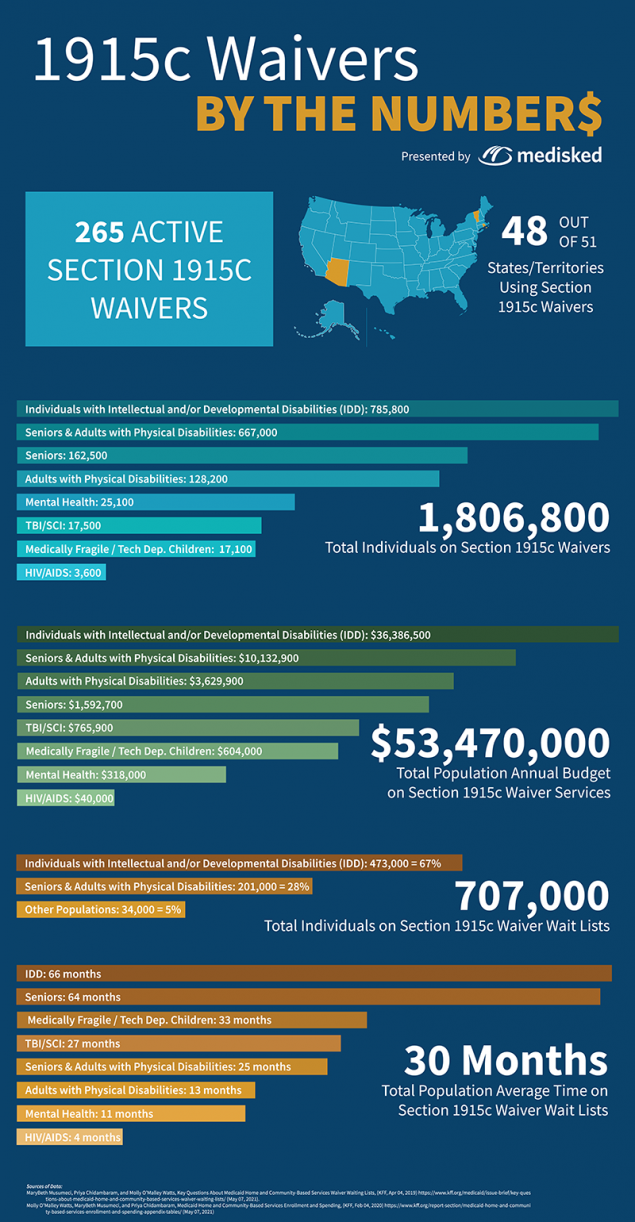
 Stephanie Crouch is a Solutions Owner specializing in state government at MediSked, the leading brand in holistic solutions that improves lives, drives efficiencies and generates innovations for human service organizations that support our community. Previously, Stephanie worked in state government for seven years as a home and community based services program manager in Nebraska where she managed the administration of 1915(c) Waivers, the Program for All Inclusive Care for the Elderly (PACE) and the state plan Personal Assistance Service. She graduated from the University of Nebraska-Lincoln with a degree in Communications.
Stephanie Crouch is a Solutions Owner specializing in state government at MediSked, the leading brand in holistic solutions that improves lives, drives efficiencies and generates innovations for human service organizations that support our community. Previously, Stephanie worked in state government for seven years as a home and community based services program manager in Nebraska where she managed the administration of 1915(c) Waivers, the Program for All Inclusive Care for the Elderly (PACE) and the state plan Personal Assistance Service. She graduated from the University of Nebraska-Lincoln with a degree in Communications. Diedra Kirk, MediSked Connect Exchange Product Manager, joined MediSked last year with nearly 20 years of product management experience. Diedra’s primary focus at MediSked is providing our clients a centralized data, reporting, and quality measurement solution.
Diedra Kirk, MediSked Connect Exchange Product Manager, joined MediSked last year with nearly 20 years of product management experience. Diedra’s primary focus at MediSked is providing our clients a centralized data, reporting, and quality measurement solution.